Extended Medicaid coverage for new moms is still alive in the state Legislature, but barely. Sen. Kevin Blackwell, R-Southaven, on Tuesday invoked a legislative maneuver that could revive his bill to extend Medicaid coverage from 60 days to a year postpartum. Speaker Philip Gunn, R-Clinton, had effectively killed the bill earlier this month , despite […]
Data: What do women in the South earn compared to men in 2022?


Mississippi is the only state to still not have an equal pay law, though it’s possible that will change soon.
House Bill 770 and Senate Bill 2451 include language that would provide legal recourse for employees being paid more or less than their counterparts of the opposite sex for the same work. A combination of both pieces of legislation will likely be passed into law before the legislative session concludes this week. However, Mississippi Black Women’s Roundtable, a Black women’s group, criticized these proposals in late January for “glaring flaws” that would still allow employers’ loopholes to legally pay women less, among other things.
View the most current data on the gender pay gaps in the Southern United States:
!function(){“use strict”;window.addEventListener(“message”,(function(e){if(void 0!==e.data[“datawrapper-height”]){var t=document.querySelectorAll(“iframe”);for(var a in e.data[“datawrapper-height”])for(var r=0;r<t.length;r++){if(t[r].contentWindow===e.source)t[r].style.height=e.data["datawrapper-height"][a]+"px"}}}))}();
WATCH: Black Women’s Roundtable discusses equal pay bills
In Mississippi, there is a 22.6% difference between the earnings of full-time, year-round working women and men in the state. That also translates to a difference of $9,755 for the average annual salary. Some places unlike Mississippi have significantly bigger monetary differences despite ultimately having smaller percentage pay gaps.
For example, Virginia’s gender pay gap in dollars is $12,442. But, because women and men in Mississippi earn, on average, less than Virginians, the smaller dollar amount difference in the gender pay gap here still creates a bigger percentage change.
Quick math: Gender pay gaps compared
Mississippi
Women earn:
$33,323/year
Men earn:
$43,078/year
Monetary pay gap:
$9,755
Percentage pay gap:
22.6%
Virginia
Women earn:
$48,439/year
Men earn:
$60,881/year
Monetary pay gap:
$12,442
Percentage pay gap:
20.4%
READ MORE:
• Mississippi Legislature passes equal pay bill. Advocates say it’s terrible
• What do Southern women make compared to men in 2021?
The post Data: What do women in the South earn compared to men in 2022? appeared first on Mississippi Today.
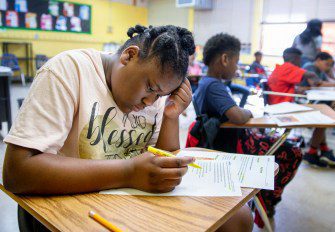
Schools will receive grades this year, prompting mixed reactions from administrators

For the first time in two years, public schools will be graded on student performance, prompting excitement from some school leaders and frustration from others who are concerned about how COVID learning loss will be represented in the data.
Public schools in the state receive A-F letter grades through what MDE calls its accountability model. It measures elementary, middle and high schools on a variety of factors including student performance and improvement in tested subjects like math and reading, as well as growth during the school year, and graduation rates.
In the spring of 2020, public schools across the state were closed because of the pandemic and state tests were not administered. The following school year, schools and districts were granted a waiver so that state tests would still be administered, but students would not be required to pass them and districts would not be graded on their performance. Results from that school year saw a decrease in the number of students passing, the first snapshot of how learning was impacted by the pandemic.
Mississippi public schools will receive grades for this school year because of efforts by Gov. Tate Reeves and the federal government to return to pre-pandemic norms.
At the March State Board of Education meeting, Mississippi Department of Education (MDE) officials said it was their goal to minimize changes to the accountability model, so that test scores and grades could be compared to their pre-pandemic counterparts as much as possible.
Ken Barron, superintendent of Yazoo County Schools, wishes the adjustments to the accountability model had been decided sooner.
“It’s frustrating to be having this conversation in March,” he said. “I’m an old coach, and I knew before the game started how they were going to assess who won the game. I didn’t get into the fourth quarter before they explained the rules to my team.”
The calculations of school grades this year must be adjusted slightly to address the missing data from 2019-20; MDE has proposed using data from before the pandemic to fill the gap. The suggested adjustment is currently available for the public to review and offer comment on.
“I appreciate the Department of Education opening it up for public comment and listening to the teachers, parents, and administrators,” said Alan Lumpkin, superintendent of the Pearl River county school district. “They’re the ones that have been on the front lines during this pandemic, and they’re the ones that are being measured.”
Lumpkin said he believes schools should be graded on student performance this year but would like to see this year’s scores used as a baseline moving forward, rather than compared test scores from before the pandemic. In his eyes, the state is in a new era of education that should require some re-examination of how the accountability model functions.
Todd English, superintendent of the Booneville School District, also believes that it is time to return to state testing, but wants communities to take the new letter grades “with a grain of salt.” Since a portion of the accountability model is based on growth, it incorporates data from prior school years to measure that growth.
“It’s going to take a couple of years for this to work itself out mathematically where the public can determine the effectiveness of a school based on letter grades,” English said. “The formula doesn’t account for a pandemic.”
English explained that elementary and middle schools will likely show strong growth this year compared to 2020-2021 scores, but that the level of growth will be difficult to maintain moving forward. He anticipates that high schools will have the opposite problem, since their growth will be compared to pre-pandemic test scores in some areas. This will likely make it difficult to show growth at all because of the learning loss that has occurred.
“MDE is in a no-win situation,” English said. “There’s not a right answer, there’s not an easy answer, there’s really not an equitable answer available.”
Adrian Hammitte, superintendent of the Jefferson County School District, has mixed feelings about the return of schools being graded on student performance. He knows students are still struggling with COVID learning loss, but feels everyone in his district has been working diligently to overcome the pandemic-induced challenges.
“I know this may be surprising, but I’m kind of excited about having the accountability model back because we are currently an F school district,” Hammitte said. “Because of the pandemic…they didn’t provide a letter grade, and we’ve been stuck with an F label (from the 2018-19 school year). Our teachers have been working very hard with students and parents despite the challenges and for us, we’re actually excited about the opportunity to remove that F label.”
While Hammitte is excited about the school grades being assigned again, he wishes some accommodations had been made for students taking the third-grade reading assessment, since they can be held back if they do not pass. A bill passed the Senate that would have allowed this year’s failing students to move on to fourth grade with remediation, but died in the House.
”If you look at our third-grade student population, those students haven’t been in school consistently since kindergarten and we know that’s where you build their foundational skills,” Hammitte said. “I believe it’s going to be difficult for quite a few of those third-grade students to get to that (benchmark).”
Cherie Labat’s concerns about equity in the accountability model began before the pandemic. Labat, superintendent of the Columbus Municipal School District, explained that disparities in personal wealth and community economic development create different starting points for children, meaning that some districts have more work to do than others.
“You expect everybody to finish the same way, but they don’t start the same way,” Labat said.
Labat had been hoping that the pandemic would provide a push to innovate the accountability system, allowing a variety of stakeholders to be brought into the conversation. She understands that MDE has been working diligently on accountability issues, but was disappointed that the model was not more broadly re-examined.
“You’re really putting a negative stamp on the students, community, and businesses, and we have to understand that when we do that, we’re not making the community move forward, we’re regressing, and regressing the areas that need economic and community development the most,” Labat said. ”A superintendent can’t descend on a school district and fix it by themselves. … The journey to get districts where they need to be for the students and families that they serve, it’s an audacious task.”
The post Schools will receive grades this year, prompting mixed reactions from administrators appeared first on Mississippi Today.
Mississippi Legislature passes equal pay bill. Advocates say it’s terrible

If Gov. Tate Reeves signs House Bill 770, Mississippi will no longer be the only state without an equal pay law on the books.
“This is a very historic day for the House, and for the state of Mississippi,” said House Judiciary A Chairwoman Angela Cockerham, I-Magnolia, lead author of the bill. “This has been a journey … over years … I think we have a very comprehensive, substantive bill.”
But some advocates of equal pay for women say the measure Mississippi lawmakers just passed is worse than not having a law and they’ll urge Reeves to veto it.
Attorney General Lynn Fitch, who has for years championed an equal pay for women law, praised its passage Wednesday after years of such measures dying, often without a vote, in a male-dominated Legislature. She said, “We will take a giant leap forward in closing the twenty-seven percent pay gap – a pay gap that makes it harder for working women and their families …”
Federal law already provides equal pay rights, but taking an employer to task in federal court is a more difficult, and often more costly task for aggrieved employees than going to state court.
One women’s advocacy group said it will urge women to continue using federal law and courts if Reeves signs HB 770 into law.
“This bill actually codifies discrimination against women for being caregivers, working mothers,” said Cassandra Welchlin, director of the Mississippi Black Women’s Roundtable. “If a woman takes off for being pregnant or caring for a child it punishes her, would allow her to be paid less, without supportive policies of maternity leave, breastfeeding, care giving.
“This will by far be the worst law in the country,” Welchlin said. “We plan on sending the governor letters urging him to veto the bill.”
VIDEO: Black Women’s Roundtable discusses equal pay bills
As lawmakers haggled out differences between House and Senate equal pay measures this session, Welchlin’s group and others pointed out what they said were glaring flaws in the proposals. Most of those remained in the final compromise bill passed Wednesday. These include:
- It would allow an employer to pay a woman less based on her “salary history or continuity of employment history demonstrated by the employee as compared to employees of the opposite sex.” This, critics say would actually allow pay discrimination against working mothers who take maternity or caregiver leave.
- It would require a woman to waive rights to a federal claim if they bring a state claim.
- It would provide less damages — only back pay and legal costs — than under federal law and includes no retaliation protection for women who file claims.
- It would apply only to full-time workers and employers with more than five employees.
House and Senate negotiators did remove one part of the bill equal pay advocates had criticized — requirements of “pleading with particularity” — a high burden of proof for employees.
Senate Judiciary A Chairman Brice Wiggins, R-Pascagoula, and Sen. Nicole Akins Boyd, R-Oxford, defended the final version sent to Reeves.
“We believe we have a good, fair bill,” Boyd said. “We worked very hard with a number of women’s groups, the business community, and had open, public conference committee meetings. I believe this is a good step in the right direction.”
Wiggins, presenting the bill to the Senate for a final vote, fielded questions about fears of “frivolous” lawsuits and other issues. “This is an extremely business friendly bill, and also will put women in Mississippi on the same level as every other state in this country … Just creating a state cause of action, that’s all it’s doing, like if you have a slip-and-fall, you’re allowed to have a civil action.”
READ MORE: Will Mississippi continue to short-change women on equal pay?
Fitch in her statement Wednesday called the measure “a critical first step” for the Legislature.
“I am grateful for the leadership of Mississippi’s Legislature in demonstrating that Mississippi values the contributions of women in our workforce, in our communities, and in our work to advance our great State to its best tomorrow,” Fitch said. “I am grateful to Representative Cockerham, Senator Wiggins, Senator Boyd, and all the legislators who supported this effort and helped prepare this bill for the Governor’s signature.”
Recent studies show women make up 51.5% of the population in Mississippi and nearly half of its workforce. They are the primary breadwinners for a majority — 53.5% — of families in this state, which is the highest rate in the nation.
But women working full time in Mississippi earn 27% less than men, far greater than the 19% gap nationwide. That gap grows worse for Black and Latina women in Mississippi, who are paid just 56 cents and 54 cents, respectively, for every dollar paid to white men.
Women make up nearly 60% of those in Mississippi’s workforce living below the poverty line. The state has continually ranked worst or near-worst in most every ranking for working women.
Women make up 16% of the 174-member state Legislature.
READ MORE:
• Data: What do women in the South earn compared to men in 2022?
• Equal pay for women: Is this the year Mississippi will join rest of the nation?
The post Mississippi Legislature passes equal pay bill. Advocates say it’s terrible appeared first on Mississippi Today.
‘From the ground up’: How one community-run program is getting more kids to college

Maple Smith has lived all her adult life in Greenville, save for the four years she spent in undergrad at Mississippi State University. A secretary in the city clerk’s office, she looks for ways to, as she puts it, “sow seeds” in Greenville in her free time — which she has a lot more of, now that her three kids have graduated college.
In 2018, the mayor’s office invited Smith to join a new initiative called the Greenville College Access Network that would help local students get financial aid for college. The idea was if more local students are able to go to college, more businesses will be attracted to create better-paying jobs in Greenville, said Mayor Errick Simmons.
Almost three years later, Smith can’t count the number of hours she’s spent helping students in Greenville apply for financial aid. Along with her co-coordinator, Sheila Watson, she’s created PowerPoints and pamphlets to help students navigate the tedious Federal Application for Student Financial Aid. The two women have made a marked difference in the number of students in their community who get college financial aid: This year, FAFSA applications at Greenville High School have more than doubled, according to Get2College.
“We started this out from the ground up,” Smith said.
The price of tuition is one of the biggest barriers to college access in Mississippi. As the Legislature has cut funding for higher education, universities across the state have steadily increased tuition. The cost of college now eats up about a quarter of annual income for working class families in Mississippi. That has an impact on college-going rates across the state and in Greenville specifically, where in 2020, 19% of adults over 25 have a bachelors compared to the national average of 33%.
In recent years, the Mississippi Office of Student Financial Aid has worked to increase the number of low-income students who get the Higher Education Legislative Plan for Needy Students, or HELP, grant which pays for all four years of college. Despite the effectiveness of the HELP grant, the Post-Secondary Board, which oversees state financial aid, cited the program’s growing cost as a reason to overhaul it.
Last year, the board proposed a new policy that would have led to Black and low-income students receiving less financial aid. The policy was created by a panel of financial aid officers at universities and colleges across the state, without input from students or parents like Smith and Watson — who know firsthand the life-changing effect the HELP grant can have on students.
“It’s imperative that students take advantage of the HELP grant,” Watson said.
READ MORE: Here’s how to apply for the FAFSA
Before GCAN formally launched in April 2021, the mayor’s office invited Smith, Watson and other local parents and high school students to participate in a brainstorming session to identify the problems that prevent students in Greenville from attending college. The session was led by Carol Cutler White, a professor at Mississippi State University who won the initial grant from the Corporation for National and Community Service that supported GCAN’s efforts.
There is no public transportation in Greenville, so it can be hard for parents to attend college nights at local high schools. And some parents might be working. Internet access is spotty, which can make it difficult for students and parents to fill out the electronic version of the FAFSA. The pandemic only made that harder, Watson said, when many parents were laid off and lost the WiFi access their jobs provided.
“COVID really put a damper in our community, and our graduation rates were really low,” Watson said. She felt like students were “giving up on going to college.”
Ideally, local high schools would offer the services that GCAN is providing. But counselors, overworked and underpaid, often don’t have time to help students apply for financial aid, Smith said. Even though she had put three kids through college, Smith had never heard a counselor mention the HELP grant.
“Until I started working with Greenville CAN — and this goes to show you how little information we are given sometimes — I knew nothing, nothing, about the HELP grant,” Smith said. “Just imagine if I had known anything about the HELP grant.”
“That’s why now when I talk to these children, and I talk to these parents, I drill into them — I drill, I drill, I drill — the HELP grant,” Smith added, “because that’s one grant that has been withheld from us for far too long.”

Every Monday and Wednesday at 5 p.m., and twice a month on Saturday, Smith and Watson man a table at the Percy Memorial Library, a public library in downtown Greenville. When GCAN started in April, they’d wait for hours only for no one to come. But word soon spread as Smith and Watson enlisted volunteers through local fraternities and sororities and churches. As more students showed up, they’d refer their friends to Smith and Watson.
Now, the two women hear from so many students who want help with the FAFSA that they’re fielding requests at all hours of the day. At 7:30 p.m. on a recent Friday night, Smith was planning to help a student fill out the FAFSA over Zoom. She’s heard from two students already in college who wanted her help talking to the financial aid office.
Over the next year, Simmons said the mayor’s office plans to grow the initiative, including changing its name to the Greenville College Access and Attainment Network.
Adding the word “attainment” signals a commitment by the mayor’s office to bring students back to Greenville after they graduate college, Simmons said. The network will also expand to support that goal: White, the MSU professor, has a new grant from AmeriCorp that will add 15-20 GCAN members to work as mentors to students — essentially formalizing the work that Smith and Watson are doing now.
Like Smith, Watson was born and raised in Greenville but left to go to college at Mississippi Valley State University. She worked in adult education under the Mississippi Department of Labor. Now Watson teaches English language arts at Weddington Elementary, where she graduated from sixth grade.
Watson has seen the difference a post-secondary degree of any kind can make in a student’s life. Her hope for students is once students get a degree, they will come back to Greenville like she did.
“It’s up to the student … to give back to their community first before they go other places,” Watson said. “That’s what we’re seeing now: Students helping, giving back to the family first.”
Editor’s note: Get2College is a program of the Woodward Hines Education Foundation, a Mississippi Today donor.
The post ‘From the ground up’: How one community-run program is getting more kids to college appeared first on Mississippi Today.
Mississippi’s largest hospital and insurer ‘not optimistic’ about reaching an agreement, leaving families in impossible positions

Brittany Brown of Madison was on the way to a photo shoot for her newborn son when she got a phone call from the state health department. There was something abnormal in her baby’s newborn screening.

Since that day a year and a half ago, Brown and her husband have lived in uncertainty. Their son was diagnosed with Pompe disease, a rare genetic condition that causes muscle weakness and progressively gets worse.
The first uncertainty came after the call: What is Pompe disease?
“I’ve never had a feeling like that,” she said. “… there’s no comparison to getting a call and Googling something like that and thinking that’s what your situation is when you thought you just birthed a healthy child.”
The Google search produced even more uncertainty. There were two types of Pompe Disease, one more severe than the other, she learned. Which did he have?
“We lived in this limbo for a few weeks waiting to find out what kind he had,” Brown recalled.
Her days now are devoted to making sure her son doesn’t fall behind in his specialist appointments and twice-monthly, $20,000 infusions that ensure he is able to walk, swallow and perform other basic tasks. His weekly visits to a physical therapist and an occupational therapist are critical, and his doctors keep a close eye on his health – any regression that goes unaddressed could quickly become permanent.
And in recent weeks, she’s been dealing with yet another unknown.
The University of Mississippi Medical Center, where her now 18-month-old sees a slew of specialists and therapists and receives his life-saving medicine, is battling with her family’s insurance company, Blue Cross Blue Shield. If the two don’t reach an agreement by Friday, UMMC will go out of network with the company – meaning Brown and her husband could face massive bills or be forced to go out of state for their son’s care.

Brown, and many other patients who either can’t or won’t go elsewhere, have not been able to get an estimate from the hospital of what their out of pocket costs would be if they continued with their UMMC providers. Brown said her son’s UMMC therapists are so wonderful, and so hard to get in with, that she is considering paying out of pocket to keep her son’s spot.
But she said she’s been told they can’t give her any idea of what the costs would be until after UMMC is officially deemed out of network with the insurance company.
Brown’s son is one of tens of thousands of Mississippians who will be impacted if UMMC and Blue Cross Blue Shield don’t settle on the terms of their contract. The dispute between the two stems from disagreement over reimbursement rates and Blue Cross’ quality care plan, which measures hospital performance and whether services provided to patients are adequate.
The public battle is a classic he-said, she-said: UMMC officials say they are only asking for the insurance company to reimburse at “under market rate” prices compared to other academic medical centers. Blue Cross leaders see it a different way.
“Blue Cross & Blue Shield establishes payment rates on the market rate for Mississippi, not what out-of-state providers are paid,” said Cayla Mangrum, manager of corporate communications for Blue Cross Blue Shield of Mississippi. “UMMC is asking for an overall 30% increase for all of its hospitals and all of its providers. Think about it this way: UMMC is asking that a nurse practitioner in a UMMC Clinic in every city in the state be paid more than every non-UMMC nurse practitioner. UMMC is asking that a physician at UMMC – Grenada be paid more than the physician at any Baptist hospital …”
But those at UMMC maintain their physicians should be treated differently than other hospitals. UMMC treats the sickest of the sick and is home to the only children’s hospital, the only Level 1 trauma center, and the only organ, tissue and bone marrow transplant program in the state.
“Blue Cross wants to compare us to other Mississippi hospitals, but there are no hospitals in the state like us,” said Dr. LouAnn Woodward, vice chancellor for health affairs and dean of the School of Medicine. “Every day we treat patients across Mississippi, many with nowhere else to turn, because they need the specialty physicians found only here at UMMC.”
But for the Mississippians who rely on those specialized services, disagreements between hospital and insurance executives don’t mean much to them. Their concern is how and whether they and their children will receive life-saving care without going bankrupt – and leaders at both UMMC and Blue Cross are aware of that.
“Unfortunately the patients are caught in the middle of this dispute,” said Dr. Alan Jones, associate vice chancellor for clinical affairs at UMMC.
Lanier Craft of Brandon also has a son with Pompe disease. For eight years, beginning with his diagnosis at three months old, mother and son have trekked to UMMC for appointments with specialists in Ear, Nose and Throat, complex care, cardiology, pulmonology, orthotics, ophthalmology, neurology and surgery.

Her son Townes receives the same infusions of medicine as Brown’s son – except he gets them weekly. Townes is also wheelchair bound, has a tracheostomy tube and is on a ventilator – making the prospect of regular trips three hours away to New Orleans, Birmingham or Memphis even more daunting.
“The truth is we can’t go anywhere else,” said Craft, crying. “This is all there is for us. Batson has been there since I walked in the door in February eight years ago with my child. They have done everything for us, and to just completely lose that within a day because of an agreement over money is unimaginable.”
Craft, a teacher, said the past week has been a frenzy. Her son has always been on her husband’s commercial plan, and if she tried to switch him to her state plan, he would either not be accepted because of a pre-existing condition or be extremely expensive.
She took half a day off work Tuesday to make phone calls: to doctors; Blue Cross Blue Shield of both Mississippi and Tennessee, the state her family has insurance through; the insurance commissioner; and any connections she has with offices and agencies who might help.

The calls got her nowhere, she said – a similar outcome reported by others who spoke to Mississippi Today. Several reported they would call UMMC’s help line only to be told to call Blue Cross. Blue Cross would then tell them they would have to call UMMC.
Around 2 a.m. Wednesday morning, Craft was awake with her son, who was struggling to maintain healthy oxygen levels. Waking in the middle of the night to tend to a health issue with the eight-year-old is common for her.
“My first thought was ‘I can’t take him to the hospital, I don’t know if he’s going to be covered,’” she said. “The first thought as a parent (in that situation) should not be ‘How am I going to afford this?’”
The fallout between the insurance company and the state’s only safety net hospital does not just impact Mississippians with rare, complex conditions.
One mom of four who spoke to Mississippi Today but did not wish to use her name in the story has spent the last three months fighting to figure out why her daughter is so sick.
After an eight-day hospital stay and a diagnosis of Kawasaki Disease last year, her daughter began developing unexplained sores. Despite multiple treatments recommended by specialists at Children’s of Mississippi, they didn’t improve. Her hair began falling out and she lost weight.
Her daughter’s pediatrician and UMMC dermatologists ran tests for various infections, but all came back negative. The doctors last week directed her to Children’s of Mississippi for a biopsy.
She scrambled to get her daughter in for the procedure before Friday, April 1, when UMMC will be considered out of network. It is scheduled for Thursday – just one day before the deadline for a contract agreement.
But regardless of the biopsy results, her daughter will still need care at UMMC – and the insurance dispute has added another layer of stress to an already stressful situation, she said.
“We will do whatever we need to do, but we only have so much savings,” she said, noticeably emotional. “One of her bills was $79,000 from when we were in the hospital… and Blue Cross paid $78,000 of that. So what else are we supposed to do?”
Because Blue Cross and UMMC have had similar public disputes in the past, some patients remain unphased, believing they will work it out as they have done before.
But while Blue Cross and UMMC disagree on a lot, they both agree on one thing: the chances of this getting worked out before April 1 are slim.
“We at UMMC don’t believe it’s going to get worked out,” Jones told Mississippi Today on Tuesday. “We’ve seen no good faith effort by Blue Cross to try to negotiate with us.”
Leaders at the insurance company said they are “not optimistic” an agreement will be reached before the deadline, but maintain they have been working to reach an agreement with the hospital.
“The fact we have not agreed to their reimbursement or quality demands does not mean we have not acted in good faith,” said Mangrum. “Since early 2021, we have had a dedicated team meeting with UMMC personnel and evaluating the financial impacts of reimbursement demands as well as quality improvement programs under which UMMC could have received additional payments if they met certain criteria.”
The post Mississippi’s largest hospital and insurer ‘not optimistic’ about reaching an agreement, leaving families in impossible positions appeared first on Mississippi Today.
Mississippi legislators want to save money on prisoners’ health care. Reluctance to expand parole makes that tricky.

Reluctance to expand parole may have led Mississippi legislators to unwittingly sabotage an effort to save state money by shifting some incarcerated people’s health care costs to Medicaid.
The state’s prisons are overcrowded, and hundreds of prisoners are sick and elderly– the consequence of harsh mandatory sentencing laws that have led to large numbers of people growing old in prison for the first time in American history.
Though many of them are eligible for Medicaid coverage because of age or disability, the program won’t pay for health care provided inside institutions like jails and prisons, leaving Mississippi on the hook for expensive health care.
The state spent about $77 million on health care for people in prison custody in 2020, including $24 million on offsite care at hospitals. Just over 500 prisoners are older than 65, and research shows the cost of incarcerating an elderly person is about three times higher than a younger person because they have much more expensive health care needs.
House Bill 936 was approved by both chambers this week and is on its way to the governor for his signature. It aims to address prison health care costs by creating “special care facilities” that could serve as a home for some of the 600 Mississippians who have been paroled but have nowhere to go and so remain in Department of Corrections custody. The bill would also expand medical parole for “medically frail” incarcerated people to the private facilities, where supporters say Medicaid would help pay for care.
The legislation could put Mississippi at the vanguard of states experimenting with placing elderly, sick incarcerated people in nursing homes.
But there’s a wrinkle: Federal guidance issued in 2016 says Medicaid won’t pay for nursing care if residents’ freedom of movement is restricted or if the criminal justice system retains a role in their health care. Some provisions of HB 936 appear to run afoul of those rules, raising the possibility that Medicaid would refuse to pay for at least some parolees’ care at the facilities, forcing the state to keep paying.
The bill defines “medically frail” as people who are so ill that they can’t perform daily living activities and are not expected to recover. Those parolees must agree to have their medical records sent to a county prosecutor every quarter if the prosecutor requests them.
And in a provision that was added after the bill passed the House and included in the final conference report, the State Parole Board will revoke parole if the person recovers, “and the department shall ensure that the inmate returns to incarceration.”
Gov. Tate Reeves’ office did not respond to a request for comment on the legislation.
Dan Mistak, acting president and director of Health Care Initiatives for Justice-Involved Populations at the non-profit Community Oriented Correctional Health Services, said sending someone back to prison if their health improves seems to cross the line Medicaid has drawn.
“A revocation like that, it signifies that you’re still under control of the state,” Mistak said.
The provision requiring parolees to agree to share their medical records with prosecutors could also compromise “personal privacy and confidentiality” of clinical records, which is a right that facilities must respect if Medicaid is to pay for care.
“They’re trying to figure out a way to still keep people under their control while at the same time trying to cost-shift to the federal government,” Mistak added.
Rep. Otis Anthony, D-Indianola, is a member of the Corrections Committee and worked on the bill.
“In order to get it passed, sometimes the other house will put in some language that will appease, you know, voters who don’t want to see people paroled for anything,” he said. “So that’s probably one of those provisions that the Senate stuck in there to ensure that they will serve their time… But for the most part I don’t think that provision will ever be used. Very few terminally ill people who will need either long-term care or hospice care will ever recover.”
Bill author Rep. Kevin Horan, R-Grenada, said that if the Centers for Medicare & Medicaid Services (CMS) doesn’t approve reimbursement for parolees’ care at the facilities, legislators can revise the law accordingly.
“I’m not saying it is a work in progress moving forward, but we gotta get something on the books, see what CMS is gonna do,” he said. “We have to do something.”
The state’s existing conditional medical release policy is used rarely. Only three people were granted the release in 2021, following seven in 2020 and 10 in 2019, according to the Department of Corrections.
Horan emphasized that the revocation provision doesn’t apply to the Mississippians who have already been paroled but remain in MDOC custody. Their parole would not be contingent on their health status, Horan said.
Sen. Daniel Sparks, R-Belmont, focused on those people while presenting the conference report on the Senate floor Tuesday afternoon.
“They have nowhere to go,” Sparks said. “Their family may have died. But they’re in MDOC. Which is a problem for us as a state. We are paying for their medical, we are paying for their housing.”
Even if Medicaid doesn’t pick up the tab at the special care facilities, the bill will save Mississippi money because paying for nursing care is cheaper than repeatedly sending a person to the hospital and paying for separate services, Sparks said on the Senate floor.
Sen. Angela Burks Hill, R-Picayune, questioned Sparks about how much the legislation would cost the state. Sparks said it would save money, but he couldn’t say how much.
Hill said she wanted to see such an estimate “before we commit to this Medicaid expansion.”
“Because that’s what it is,” she said. “It’s Medicaid expansion for prisoners and parolees.”
Hill and 15 other senators voted against the conference bill.
Many Republicans who don’t support expanding Medicaid for working-poor Mississippians voted in favor of HB 936. Sen. Brice Wiggins, R-Pascagoula, sponsored a separate bill, SB 2448, that would have also created the “special care facilities” for medically frail inmates. In an interview with Mississippi Today, he declined to explain why he doesn’t support Medicaid expansion in general.
His bill passed the Senate with broad support before dying in the House Medicaid Committee. Wiggins also participated in the conference on HB 936.
The legislation makes Mississisppi part of a growing wave of states trying to figure out ways to use Medicaid to help reduce the costs of providing health care for incarcerated people.
Mistak said Mississippi is unusual because most states that have pursued that goal expanded Medicaid eligibility based on income. That creates greater potential savings, because it makes almost every incarcerated person eligible. Then the program will pay for care that requires a hospital stay of at least 24 hours.
There’s still not much precedent in other states to show how exactly Mississippi’s program would play out if enacted. In Connecticut, a nursing home called 60 West houses people paroled from prison following a 2013 law. But Medicaid initially refused to reimburse Connecticut for parolees’ care there, citing the presence of security measures that had no medical justification. After the facility made changes, Medicaid agreed to pay. Today, 60 West looks like any other nursing home.
David Skoczulek, vice president of business development at iCare Health Network, which operates 60 West, told Mississippi Today that a handful of 60 West residents have returned to prison after violating a term of their parole. But no one living at 60 West can be returned to prison simply because their health improved.
“It would seem to be extraordinarily difficult to protect resident rights in a way that conforms with CMS rules and requirements if they still require the types of custody precautions of a current prisoner,” he said.
The facility does not share medical records with anyone in the corrections or justice system, he added.
HB 936 would also create regulations for the special care facilities, and stipulates that there can be no more than three in each Supreme Court district. MDOC would be responsible for contracting with the facilities and would regulate them along with the Department of Health.
The post Mississippi legislators want to save money on prisoners’ health care. Reluctance to expand parole makes that tricky. appeared first on Mississippi Today.
Tupelo couple sues north Mississippi hospital for alleged balance billing

A Tupelo couple is suing a north Mississippi hospital and its affiliates over an alleged balance-billing scheme that cost them nearly $50,000.
Balance billing is illegal under a state law passed in 2013. The law states that if a health care provider accepts payment from a health insurance company on behalf of a patient, the provider is prohibited from collecting any amount from the patient above their deductible, co-pay, or co-insurance amount.
For example, if a patient is billed $10,000 by their hospital the health insurance company pays the hospital $5,000, and the hospital cannot then try to collect the remaining $5,000 from the patient.
Though balance billing is illegal in Mississippi, it still happens, as many are still unaware of the state law.
In 2017, Chastity Woods needed dozens of non-elective medical treatments, including blood and iron transfusions, according to the lawsuit. She received these treatments from North Mississippi Medical Center (NMMC) in Tupelo and local clinics also owned by the hospital’s Delaware-based parent company, North Mississippi Health Services, Inc.
After receiving payment from Chastity’s insurer Health Cost Solutions, the providers returned to the Woods to demand nearly $50,000 in additional payments in 2018.
Unaware of Mississippi’s ban on balance billing, the Woods accepted a special “tax time deal” from the debt collectors in March 2019 that would reduce their bills by 20%. They then paid the bills by taking out a home equity line of credit, the suit states.
The Woods allege that the debt collector came back in October 2019 to demand an additional $8,936.05 – even after the Woods paid nearly $42,000 to the hospital and debt collector. The Woods allege that the debt collectors continued to harass them until they filed their lawsuit in Feb. 2020.
Chastity declined to speak to Mississippi Today for the story. Calls to their attorney were not returned. Bruce J. Toppin, chief legal officer at North Mississippi Health Services, told Mississippi Today that the company does not comment on pending litigation.
Though balance billing is against the law in Mississippi, some hospitals haven’t updated their business models since the law was passed, according to Roy Mitchell, executive director of the Mississippi Health Advocacy Program.
“We (Mississippi) have the highest rate of medical debt in the country. We have for years … And (balance billing) is all based on a business model that, unfortunately, some providers are still clinging to,” Mitchell said.
The ban on balance billing is largely toothless, with Insurance Commissioner Mike Chaney and Attorney General Lynn Fitch claiming they lack the statutory enforcement authority to take action against hospitals that break the law. This leaves patients like the Woods with no alternative to lengthy and costly lawsuits.
A legislative attempt to strengthen the balance billing law in 2019 would have required the attorney general’s office to enforce the law and establish binding arbitration to resolve any balance billing disputes between providers and patients. Though it was authored by then House Insurance Chairman Rep. Gary Chism, the bill never made it out of committee.
Chism told Mississippi Today in 2019 that lawmakers who were also medical professionals opposed the bill.
“They want to be able to get their money,” Chism said.
Because Chastity’s health insurance plan is not in NMMC’s network, the hospital would have received a higher reimbursement if she had used Stanley’s insurance, attorneys for the hospital say.
“The Woods took the cheap way out and wound up with significantly higher out-of-pocket costs as a result,” the attorneys wrote.
The Woods chose to use Chastity’s Health Cost Solutions plan instead of Stanley’s state employees plan because the former had a lower deductible. But Mississippi’s anti-balance billing doesn’t distinguish between types of networks. According to the law, as long as the provider accepts payment from the insurer, “the payment shall be considered payment in full to the provider, who may not bill or collect from the insured any amount above that payment, other than the deductible, coinsurance, copayment or other charges for equipment or services requested by the insured that are non-covered benefits.”
The Woods attorneys have argued that if the providers believed the reimbursement rates offered by Chastity’s insurer weren’t high enough, they could have refused to provide the non-emergency treatment or insisted the Woods find another way to pay. Instead, NMMC accepted at least 48 different payments from Chastity’s insurer, at 140% of the rate Medicare would have paid, the lawsuit alleges.
In addition to damages, the Woods are seeking a permanent injunction against NMMC issuing or attempting to collect balance bills.
The post Tupelo couple sues north Mississippi hospital for alleged balance billing appeared first on Mississippi Today.
WILL A JURY CONVICT HER AGAIN…?
A Hattiesburg native will be tried for murder a 2nd time in the death of her stepdaughter.
T’kia Smith Bevily is set to stand trial a second time in Claiborne County in the murder of her 14-month-old stepdaughter Jurayah. Both T’kia Bevily and her husband, Morris Bevily, the child’s biological father, were charged in the 2017 murder. T’kia Bevily stood trial in January, 2021 and was convicted unanimously in the murder. She was sentenced to life without parole, but that conviction was vacated in September, 2021 for jury misconduct after it was discovered that a juror failed to disclose that he was related to the victim. Mrs. Bevily’s 2nd trial is set for May 2nd. Mr. Bevily’s trial is set for May 9th in Claiborne County Circuit Court. T’kia Bevily’s attorney asked for a continuance in the trial, but that request was denied by the presiding judge.
The case has drawn much attention within the Hattiesburg community, with supporters for T’kia clashing on social media with those who believe she’s guilty. The child died from multiple (as many as five) contusions due to blunt force trauma to the head, according to medical examiner reports. According to the medical examiner, and expert pathologist for the prosecution, the injuries, which reportedly occurred on the evening of October 21st or the early morning hours of October 22, 2017, resulted in the death of the child, and would have occurred while the child was in the sole care of the Bevilys.
Click here to read more on the Tkia Bevily case here.
Get caught-up at the links below:
Tkia Bevily initial interrogation
https://fb.watch/bmn_O_CiLO/
T’kia Bevily highlight from 2nd Interrogation: https://fb.watch/bmnXMjNYCb/
Morris Bevily full (2) interrogations
https://fb.watch/bmnZ4Yuarn/
Ms Bevily 1st trial transcript can be found in the group here
https://www.facebook.com/groups/hattiesburgpatriot/?ref=share
Ms. Bevily and her brother Chris went on camera to explain the reason a continuance was requested. you can watch that video here.
https://fb.watch/b5cKLDSkwv/
The Bevilys maintain their innocence in the death of baby Jurayah.
#TruthForBabyJurathe
Empower releases video on tax reform
As the Mississippi legislature adopts the largest tax cut in state history, Empower Mississippi has released a video explaining the tax reform changes.
The new law phases in the more than $500 million tax cut over the next four years. In the first year, it would eliminate Mississippi’s current 4 percent bracket that currently applies to the first $5,000 in taxed income. In years two through four, it would reduce the rate that applies to all income over $10,000 from 5 percent down to 4 percent. The end result would be a higher threshold before any taxes are owed and a lower, flat rate on all taxable income.
Empower has spent two years building the case and need for substantive tax reform in Mississippi, from issuing the first dynamic economic modeling of income tax elimination plans to testifying at joint legislative hearings, from engaging the media with over 1,000 mentions of our work to reaching the general public with millions of views of our content on the web and social media, and from designing and proposing alternate policy suggestions to activating citizens to send over 9,200 emails in support of tax reform.
The bill has been transmitted to the Governor and he has until April 5 to sign.